A new chapter for clinical trust, patient safety, and digital accountability - Across Malaysia's healthcare landscape, the humble prescription pad is quietly being replaced by encrypted digital documents. What began as a pandemic-era necessity has evolved into a nationwide effort to modernise medical prescribing with legally recognised digital signatures. Hospitals, regulators, and technology providers are now working together to ensure every prescription is authentic, traceable, and tamper-proof.
Yet the transition is far from a simple software upgrade. Behind every electronic prescription lies a complex web of law, identity management, cryptography, and clinical workflow redesign. This is the story of how Malaysia is implementing e-prescription e-signature systems — how they integrate into Hospital Information Systems (HIS), how they connect to licensed certificate authorities, how inpatient and locum scenarios are handled, and how regulatory frameworks are redefining trust in healthcare.
1. Why E-Prescriptions Matter
In traditional hospitals, the prescribing process has always hinged on paper. Doctors wrote orders by hand; pharmacists deciphered handwriting; patients carried physical slips between departments. That system, while familiar, was fragile. Prescriptions could be misplaced, altered, or forged. Errors from illegible writing and transcription led to medication mistakes.
As Malaysia pushes toward digital healthcare, the e-prescription has become more than a convenience — it is now a cornerstone of safe and accountable clinical practice. By replacing handwritten notes with digitally signed electronic records, hospitals gain three powerful advantages: integrity, traceability, and legal enforceability.
Digital signatures ensure that once a prescription is issued, it cannot be modified without detection. Each signature binds the document cryptographically to the doctor's verified identity. When pharmacists receive that prescription, they can confirm with certainty that it was issued by a legitimate prescriber and has not been tampered with in transit. For patients, this means safer dispensing; for hospitals, it means demonstrable compliance with national laws.
2. The Legal Foundation of Digital Prescribing
Malaysia's journey toward e-prescription legality rests on three legislative pillars.
The Electronic Commerce Act 2006 first established that electronic documents and electronic signatures could satisfy legal requirements for writing and signing. It opened the door for digital records in both commerce and healthcare.
The Digital Signature Act 1997 then defined the higher-trust model — a digital signature based on cryptographic certificates issued by licensed Certification Authorities (CAs) regulated by the Malaysian Communications and Multimedia Commission (MCMC). Signatures made under this Act carry the same force as handwritten ones, provided they are created with a certified private key and verified against a licensed CA.
Finally, the Poisons (Amendment) Act 2022 updated the Poisons Act 1952 to acknowledge electronic communication in pharmacy transactions. It allows prescriptions and written orders to exist electronically, but with an important caveat: prescriptions must still comply with stricter verification standards. This is where the digital-signature model becomes essential.
In practice, the Ministry of Health (MOH) interprets these laws to mean that any electronic prescription — especially those involving scheduled or controlled medicines — must be digitally signed using a certificate issued by a licensed Malaysian CA and verifiable by pharmacists before dispensing.
3. Malaysia's Certificate Ecosystem
Several licensed Malaysian Certification Authorities provide the backbone for these signatures. Each offers APIs and trust-service platforms hospitals can integrate with. While the exact provider may differ between health networks, all operate under the same regulatory oversight and technical baseline set by MCMC.
| Provider | Key Capabilities for Healthcare Use | Notes on Adoption and Integration |
| MSC Trustgate .com Sdn Bhd | Mature PKI infrastructure, enterprise-grade identity lifecycle tools, hospital-scale certificate issuance. | Common choice among large healthcare groups that require thousands of prescriber certificates. |
| Pos Digicert Sdn Bhd | Specialises in regulated industries, emphasises audit logging, timestamping, and secure key storage. | Suited to hospitals with strict internal governance or ISO 27001 frameworks. |
| Securemetric Technology Sdn Bhd ('SigningCloud') | Cloud-based signing gateway supporting remote signing via web and mobile. | Ideal for telehealth or outpatient clinics where doctors sign off-site. |
| Telekom Applied Business Sdn Bhd (TM Applied Business) | Developer-friendly APIs, competitive pricing, modular licensing. | Favoured by mid-sized private hospitals building custom HIS platforms. |
| DigiCert Malaysia (BERCA Digital Solutions) or MyTrust ID Sdn Bhd | Strong identity verification, supports short-term certificate leasing for locum doctors. | Attractive to institutions with high turnover of visiting clinicians. |
Together, these providers form the national trust infrastructure that underpins e-prescription authentication. Hospitals select based on integration ease, cost, and support for doctor identity management. Larger groups often negotiate enterprise arrangements so every prescriber — from consultants to locums — has an individual signing credential traceable to the hospital's trust policy.
4. How the E-Prescription Workflow Operates
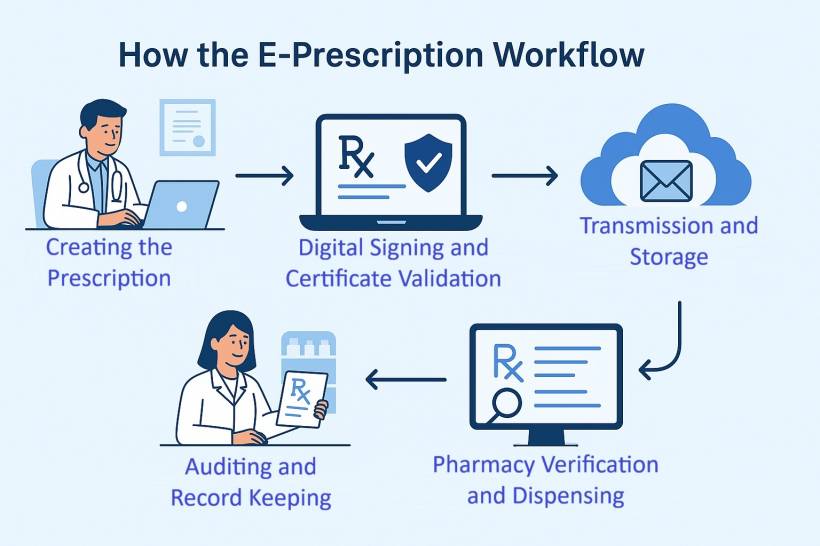
Step 1 – Creating the Prescription
Within the Hospital Information System, a doctor opens the electronic prescribing module and selects a patient record. The system already knows the patient's demographics, allergies, and current medication profile. The doctor enters the new medication order: drug name, dose, route, frequency, duration, and any special instructions.
When the doctor clicks "Confirm Prescription," the HIS assembles a structured data object. This payload includes the patient's ID, the doctor's full credentials, the hospital's licence information, the timestamp, and the list of ordered medicines. At this moment, it is an unsigned draft awaiting authentication.
Step 2 – Digital Signing and Certificate Validation
The HIS sends the draft to the hospital's internal signing gateway — a service that links the hospital system to the external Certification Authority. The gateway checks that the doctor's certificate is valid and that the doctor is actively authorised to prescribe under the hospital's credentialing rules.
The doctor is prompted to authenticate, often using two-factor confirmation. The gateway then hashes the prescription content and requests the CA to sign that hash with the doctor's private key stored in a secure hardware module. The resulting signature and certificate chain are returned to the HIS, which embeds them into the prescription file.
Within seconds, the system transforms the draft into a legally binding digital prescription. Any alteration — even a single character — would break the hash and render the signature invalid.
Step 3 – Transmission and Storage
The signed prescription is stored immutably in the HIS and simultaneously transmitted to the pharmacy information system. A secure audit record notes who signed, when, and with which certificate.
Hospitals typically maintain these signed prescriptions for years, meeting retention standards set by MOH and internal governance committees. The data is encrypted at rest and backed up to prevent loss.
Step 4 – Pharmacy Verification and Dispensing
When the pharmacy receives the prescription, its software automatically validates the signature. If the certificate chain is trusted and the document hash matches, the pharmacist can safely dispense the medication. If verification fails — perhaps due to an expired certificate or tampering — the system blocks dispensing until the issue is resolved.
This verification process has become a legal obligation. MOH's enforcement units expect pharmacists to confirm authenticity before supplying scheduled medicines. A failure to do so could expose the pharmacist and the facility to penalties under the Poisons Act.
Step 5 – Auditing and Record Keeping
Every signed prescription contributes to a verifiable audit trail. Hospital administrators can generate compliance reports showing how many prescriptions were signed digitally, which doctors issued them, and whether any pharmacist interventions occurred. This data also supports quality-improvement initiatives, allowing hospitals to monitor prescribing patterns and reduce errors.
5. Integration within Hospital Information Systems
Implementing e-prescription signing is not merely a plug-in. It requires re-architecting parts of the HIS to handle identity, workflow timing, and signature storage securely.
Each doctor must be uniquely identifiable within the HIS. Their profile links to MMC registration numbers, specialties, and employment status. When the HIS requests a certificate from a CA, it uses this verified information. Hospitals often integrate human-resources systems with the HIS to automate onboarding and off-boarding so that only active doctors possess valid signing rights.
Rather than embedding cryptographic operations directly inside the HIS, most institutions deploy a signing gateway. This middleware handles certificate validation, key management, and interaction with multiple CAs if needed. It can also enforce policy rules — for instance, restricting signing privileges for probationary doctors or interns.
Signing must feel instantaneous. A delay of even a few seconds per prescription could frustrate clinicians. Successful implementations therefore rely on asynchronous processing: the doctor signs, moves to the next task, and the system completes verification in the background while logging results.
Hospitals store only public certificates and signed artifacts. Private keys remain inside the CA's secure hardware modules. This separation reduces legal liability; if a breach occurs, the CA remains accountable for key protection while the hospital ensures secure transmission and record keeping.
6. Inpatient vs Outpatient Prescribing The Inpatient Environment
Within wards, intensive-care units, or operating theatres, medication orders are frequent and dynamic. Doctors adjust dosages and timings daily based on patient response. Because these orders are internal and administered by nurses, they fall under the category of medical orders rather than formal prescriptions under the Poisons Act.
Hospitals therefore rely on user authentication and audit trails instead of full digital signatures for every change. Each entry is time-stamped and linked to the doctor's verified login. This approach maintains accountability without slowing down urgent clinical decisions.
The Outpatient and Discharge Scenario
When medication leaves the hospital — whether as discharge medicine, outpatient pharmacy supply, or telehealth delivery — it becomes a prescription in the legal sense. Here the full digital-signature workflow activates.
The signed prescription document accompanies the patient record to the pharmacy. Pharmacists verify it before dispensing, ensuring that every tablet or vial leaving the hospital is backed by a valid digital certificate. The process satisfies both the Digital Signature Act and MOH's current enforcement expectations.
7. Managing Locum and Visiting Doctors
Locum doctors are a reality in Malaysian healthcare. They fill shifts, assist in specialised clinics, and cover weekends or holidays. In a digital-signature environment, they introduce complex identity-management challenges.
Hospitals must ensure each locum has a distinct, legally verifiable signing identity. The certificate cannot be shared or reused; doing so would invalidate non-repudiation and expose the institution to audit failures.
Modern HIS platforms therefore maintain a Doctor Identity Registry that mirrors HR data. When a locum joins, the registry requests a temporary certificate valid for the duration of their engagement. The system activates signing rights on their first shift and automatically disables them at contract end. Historical prescriptions remain verifiable because the certificate, though expired, can still validate past signatures.
This lifecycle management is crucial. It ensures every digital signature in the hospital traces back to a real, authorised individual, even if that person worked only a weekend shift.
8. Pharmacist Intervention and Revision Workflow
Digital prescribing does not eliminate the need for clinical dialogue. Pharmacists remain the last safeguard in the medication chain. When they detect a potential problem — an excessive dose, an allergy conflict, or a contraindication — they must intervene.
In the paper era, such interventions were scribbled notes or phone calls. In a digital environment, they become structured events. The pharmacist flags the issue in the pharmacy module, which sends a notification to the prescriber's queue. The doctor reviews the suggestion, edits the prescription if necessary, and re-signs the new version digitally.
Each revision creates a new immutable record. The old version remains archived, preserving a complete trail of the clinical decision process. This version-controlled workflow not only satisfies regulators but also strengthens patient safety culture inside the hospital.
9. Real-World Adoption in Malaysia
Malaysia's private sector has been at the forefront of e-prescription adoption. Large tertiary hospitals in Kuala Lumpur and Penang began pilot projects years ago, integrating electronic medication order entry with digital-signature modules. Telehealth platforms have accelerated acceptance by demonstrating scalability — some reporting hundreds of thousands of digitally signed prescriptions annually.
Public hospitals are now following suit under the broader MyDigital Health Blueprint. Pilot implementations within government facilities focus on outpatient departments, where dispensing volumes are highest. Feedback indicates significant reductions in administrative workload, fewer prescription verification calls, and improved audit readiness.
These early successes demonstrate that digital prescribing is not theoretical; it is already functioning across Malaysia's healthcare ecosystem, from online consultations to major hospital groups.
10. Regulatory Oversight and Enforcement Direction
The Ministry of Health's Pharmacy Enforcement Division plays a central role in policing compliance. Inspectors conduct spot checks on pharmacies — both community and hospital-based — to ensure that medicines are dispensed only against valid prescriptions. Under the new interpretation of the Poisons Act, an "electronic prescription" without a valid digital signature is treated as non-compliant.
Professional bodies such as the Malaysian Medical Association (MMA) support this stance, calling for tighter enforcement to curb unsafe online prescribing and ensure patient safety. Their position aligns with MOH's view that digital signatures provide the necessary assurance of authenticity in remote and telehealth contexts.
Over the next few years, the government is expected to issue more detailed technical regulations, possibly defining signature formats, certificate lifespans, and interoperability standards between hospital systems and national health records. Hospitals that have already adopted certificate-based workflows will find themselves ahead of these mandates.
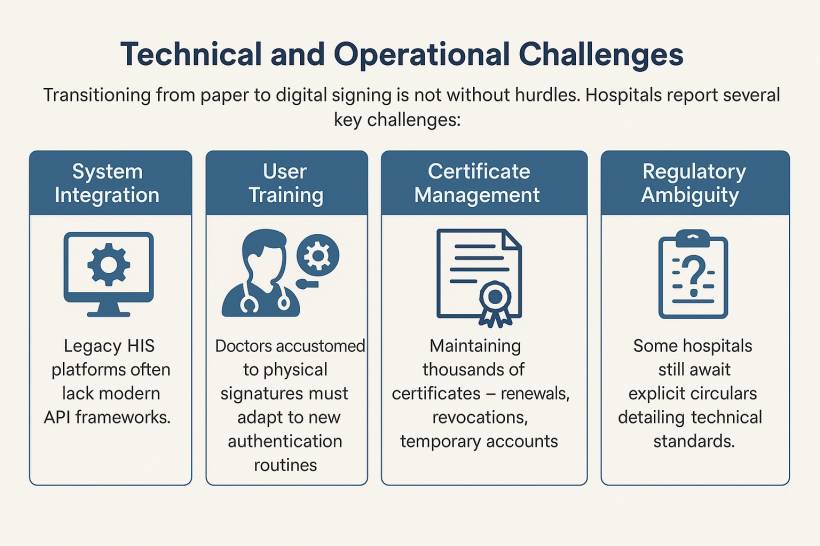
11. Technical and Operational Challenges
Transitioning from paper to digital signing is not without hurdles. Hospitals report several key challenges:
Legacy HIS platforms often lack modern API frameworks. Integrating with certificate authorities requires new middleware or upgrades to service-oriented architectures.
Doctors accustomed to physical signatures must adapt to new authentication routines. Training and user-experience design are vital to prevent resistance.
Maintaining thousands of certificates — renewals, revocations, temporary accounts — demands automated tools and clear governance. Many hospitals create dedicated "Digital Trust Administration" roles to manage this lifecycle.
Licensing digital certificates for every prescriber can be costly initially, though enterprise pricing and volume agreements help. Over time, savings in paper handling, reduced fraud, and audit efficiency offset these costs.
While enforcement bodies treat digital signatures as mandatory for e-prescriptions, some hospitals still await explicit circulars detailing technical standards. Most therefore choose to comply proactively rather than risk penalties later.
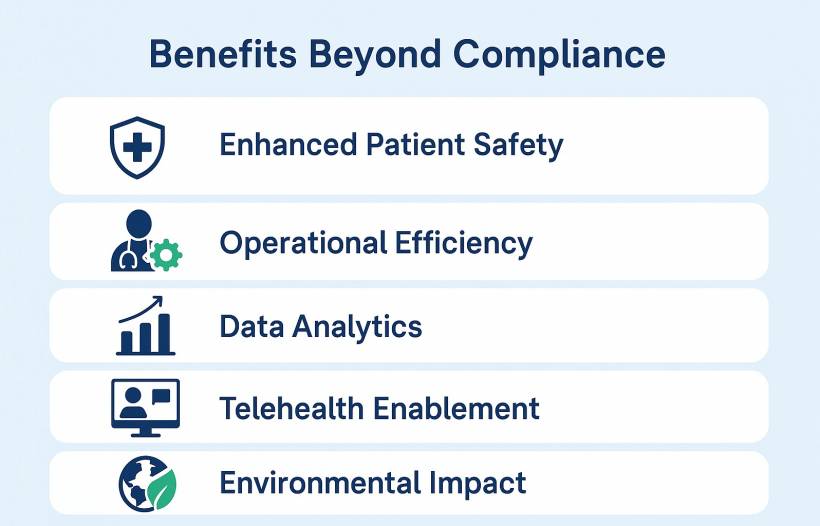
12. Benefits Beyond Compliance
Once hospitals implement digital prescriptions successfully, the benefits extend far beyond legal obligation.
Illegible handwriting and transcription errors vanish. The system can automatically flag drug interactions, duplicate therapies, and allergies before signing.
Doctors no longer chase physical forms. Pharmacists spend less time verifying signatures or clarifying orders. Prescriptions reach the pharmacy instantly, accelerating turnaround.
Digitally signed prescriptions generate structured data suitable for pharmacovigilance and utilisation studies. Hospitals can analyse prescribing trends, cost patterns, and patient adherence.
With secure digital signing, remote consultations can produce legally valid prescriptions deliverable to any licensed pharmacy. This capability proved essential during pandemic lockdowns and continues to support chronic-disease management programs.
Reducing paper prescriptions aligns with sustainability goals. Large hospitals that fully digitise prescribing save tens of thousands of sheets annually.
13. Designing for the Future: Toward a National Prescription Network
As more hospitals implement certificate-based e-prescribing, Malaysia is inching toward a connected national framework. A shared verification portal could allow any pharmacist — public or private — to validate a prescription's authenticity in real time.
Such a network would require interoperable data standards and a central registry of trusted certificate authorities. Work is already underway within government agencies to explore this concept. In time, patients could present a QR-coded prescription at any participating pharmacy nationwide, confident that the system will verify its legitimacy instantly.
This vision aligns with the government's broader digital-health objectives: unifying patient data, strengthening cyber-resilience, and enabling secure cross-institution collaboration.
14. Lessons from Implementation Projects
Hospitals that have already deployed digital signatures in prescribing share several lessons:
These lessons reflect a broader truth: successful e-prescription projects are as much about people and process as they are about technology.
15. The Role of Education and Cultural Change
Digital transformation in healthcare succeeds only when clinicians trust the system. Hospitals implementing e-prescription e-signatures must therefore invest in education. Workshops explaining how digital signatures protect doctors from forgery and misuse often shift attitudes from scepticism to enthusiasm.
Medical schools and postgraduate training programs are also beginning to include modules on digital health ethics and data governance. As the next generation of doctors enters practice, familiarity with secure electronic prescribing will become second nature — the same way electronic medical records are today.
16. Looking Ahead: Beyond Prescriptions
E-prescription is only the first step in Malaysia's broader move toward a fully digital clinical documentation ecosystem. The same certificate infrastructure can support electronic medical certificates, referral letters, imaging reports, and discharge summaries. Once a doctor possesses a verified digital identity, any document they sign can carry legal validity across systems.
In the long run, this interconnected trust framework could underpin cross-hospital data exchange, insurance claim authentication, and even AI-assisted clinical decision support, all while maintaining the same standard of non-repudiation and integrity that digital prescriptions introduced.
17. Conclusion: A New Standard of Trust
The implementation of e-prescription e-signature systems in Malaysia marks a defining moment for healthcare digitalisation. It transforms how prescriptions are created, verified, and stored, anchoring every step in cryptographic certainty and legal accountability.
For hospitals, the journey